DENTAL FACTSHEET
Horse’s teeth could hardly be more different than our own (see third picture above). They have 6 incisor teeth in the upper and lower jaws and then a large gap before the six cheek teeth. We use the term ‘cheek teeth’ to describe the premolar and molar teeth collectively. Male horses also have canine teeth which emerge at about 5 years of age in the gap between the incisors and molar teeth in both upper and lower jaws. They are only occasionally seen in mares.

- Quidding - dropping food.
- Balling – food pouches in the cheeks like a hamster
- Inappetence - reluctance to eat
- Tossing of the head or biting discomfort.
- Smaller enamel overgrowths can be easily removed with a hand rasp or ‘float’. A gag must be placed in your horse’s mouth to safely and properly inspect and rasp the teeth. About 1 in 20 horses find this frightening and require light sedation. The way to avoid this is to have your horse checked each year from two years old so that they are used to having a ‘Gag’ put into their mouth. Most horses do not need any actual rasping until they are 4- or 5-year-olds when they have all their adult cheek teeth in place.
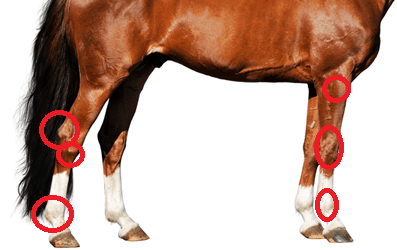
- Some horses will need these enamel overgrowths removed twice yearly. More severe overgrowths – hooks and ramps (see below) - do occur and are often caused by malformation of the teeth such that they do not have an opposing tooth to wear against.
- Hooks and ramps require motorised burrs to remove these large areas of diamond-hard enamel. They commonly recur at the same rate that the tooth is erupting, i.e., 2-3 mm per year, and so require treatment every year or so

Diastema
Diastema are caused by malformation of the teeth so that food jams between two adjacent cheek teeth. Daily grinding packs more and more food into the tiny space, eventually forcing food under the gum line. Diastema can be difficult to identify, often requiring the use of a dental mirror. The picture on the left below shows food jammed at the ‘6 o’clock’ position in the mirror.

Diastema are a common cause of oral pain and require specialist treatment to either widen the space between the two teeth, allowing the food to move freely in and out of the gap, or to extract the cheek tooth if it has become diseased.
It is important to identify diastema early as widening the space can save the tooth. The gap is widened using a special motorised burr (above right). This procedure may require repeating as the teeth grow and the gap closes.
Cheek Teeth Fractures and Abscesses
Fractures and abscesses involving the cheek teeth invariably require extraction of the offending tooth. This is a major undertaking in horses due to the massive length of the ‘root’.
Traditionally teeth were extracted by making a hole in the face (for an upper tooth) or the jaw (for a lower tooth) and hammering out the tooth. Now it is much more common to extract teeth from the mouth by using large dental extractors (below) to loosen a diseased tooth and pull it free.

Oral extractions require substantial patience as it can take 6-8 hours to wiggle the tooth loose. Great care must be taken not to fracture the tooth or leave fragments behind. The teeth at the bottom left of the picture above are from a 20-year-old horse and only a third of the length of those in 7 year-old.
Occasionally, and especially in young horses, it is not possible to extract a tooth orally. In these cases, the horse is anaesthetised and a dental punch inserted through a hole made in the jaw bone or face to hammer out the tooth. The picture on the right above shows an Xray taken during surgery to check that the dental punch is correctly positioned prior to being hammered.
Wolf Teeth
About a third of horses have wolf teeth that erupt just in front of the cheek teeth between 1 and 8 years of age. They serve no purpose and are a remnant of the first pre-molar tooth that is no longer required. About 50% of horses need to have it removed as it interferes with the bit. This is easily done under light sedation.
There are many areas not covered in this fact sheet, but we hope it has helped you understand your horse’s mouth. Horses have quite amazing teeth and a simple check-up at vaccination time should keep them that way.
If you have any further questions, please do not hesitate to contact us on